Items filtered by date: December 2020
Residency Training for Podiatrists

Podiatrists are foot specialists that can identify and treat a number of different foot afflictions, including plantar fasciitis, toenail fungus, athlete’s foot, and many others. To become a podiatrist, one must complete a rigorous residency training following completion of the curriculum in a podiatric medical school. A minimum of at least two years of residency training is mandated by many states. This training period is important for podiatrists for many reasons. Importantly, completing a residency exposes an aspiring podiatrist to a variety of different surgical and medical experiences in the real world. A residency can also prove to be an informative interdisciplinary activity, enabling the aspiring podiatrist to be exposed to surgery, anesthesiology, pediatrics, and more. If you struggle with foot pain or some kind of foot condition, do not hesitate to contact your podiatrist to make an appointment.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact Sarah Urton, DPM from Kitsilano Foot and Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our office located in Vancouver, BC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Signs of an Achilles Tendon Injury

There are different ways in which an individual may injure their achilles tendon, the tendon that runs from the calf muscle to the heel bone in the lower leg. For example, an individual can tear or rupture their Achilles tendon when it is strained or stretched beyond its limits. There are several signs of an Achilles tendon injury to be aware of. Namely, you might experience pain when walking up staircases because the Achilles tendon essentially enables you to lift your heel off of the ground. In the same vein, you could experience difficulty trying to stand on the tips of your toes. Additionally, if you have an Achilles tendon injury, you might notice different types of pain. You can experience sharp pain at the back of the ankle or leg. Snapping or cracking sounds might be heard if you have experienced some kind of Achilles tendon injury. If you suspect that you have developed this kind of injury, do not hesitate to schedule an appointment with a podiatrist, a foot care specialist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Sarah Urton, DPM of Kitsilano Foot and Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Vancouver, BC . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Diabetic Limb Salvage
Limb salvage is a procedure that involves saving a lower extremity from amputation. In podiatry, limb amputation often occurs as a result of diabetes. The fundamental goal of limb salvage is to restore and maintain stability and movement of the affected lower extremity.
The procedure typically involves removing the diseased tissue and a small portion of the surrounding healthy tissue, as well as the removal of any affected bone if necessary. If bone is removed it is then replaced with prostheses, or synthetic metal rods or plates, or grafts from either the patient’s body or a donor. Limb salvage is typically the preferred choice of procedure over amputation, as the procedure preserves both the patient’s appearance and allows for the greatest possible degree of function in the affected limb.
Upon diagnosis and determining that limb salvage is the appropriate treatment, the podiatrist may enlist the help of a physical and/or occupational therapist to prepare the patient for surgery by introducing various muscle-strengthening, walking, and range of motion exercises. Such exercises may be continued as rehabilitation post-procedure.
Foot Wounds and Diabetic Ulcers May Lead To Amputation

The amount of lower limb amputations is at an increased rate, and this is especially true of diabetic patients. High blood levels and poor glucose management can significantly contribute to the onset of diabetes which can lead to the amputation of a toe or a leg. An unnoticed cut on the bottom of the foot may lead to an infection that grows into a diabetic foot ulcer. This can be from the inability to heal properly, in addition to not keeping the weight off of the foot. There are methods that can be implemented which can help to eliminate the need for amputation. These can include controlling the body’s sugar levels, and having regular foot assessments performed by a podiatrist. Research has indicated this may help to reduce the risk of developing a foot ulcer by approximately 50%, which can lead to possible prevention of amputation. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist, who can help you to properly manage this condition, and guide you toward methods in controlling your blood sugar.
Diabetic Limb Salvage
Diabetic limb salvage can be an effective way in preventing the need for limb amputation. If you have a foot ulcer and diabetes, consult with Sarah Urton, DPM from Kitsilano Foot and Ankle Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Diabetic Limb Salvage?
Diabetic limb salvage is the attempt of saving a limb, such as the foot, that has an infected ulcer, from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
Diabetes is the number one cause of non-traumatic amputations in the United States. Amputation has been found to lead to higher mortality rates. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our office located in Vancouver, BC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Are You Suffering From Ingrown Toenails?
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Bunion Formation
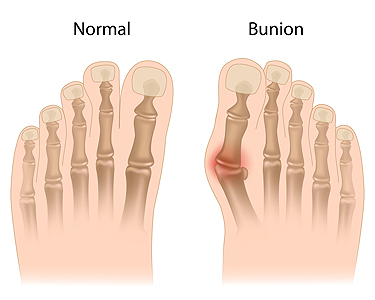
There are a number of foot conditions that you may encounter at one point during your lifetime. Some of them involve the formation of certain abnormal bony protrusions that can cause pain or discomfort. One such foot condition involving a bony protrusion is known as a bunion. Bunions typically develop on the side of the big toe, and in some cases, bunionettes might form on the smallest toe. Since bunions can be an annoyance to those afflicted by them, bunion formation and its causes are of the utmost importance. Bunions are commonly caused by ill-fitting footwear that makes the toes crowd together. Whenever an individual puts a significant amount of pressure on their big toe joint for an extended period of time, this can also potentially lead to bunion formation. Having other conditions or diseases might also lead to bunion formation. For example, having rheumatoid arthritis, cerebral palsy, and Down syndrome makes one particularly vulnerable to developing a bunion. After a bunion forms, it can cause soreness at the affected area or even swelling around the big toe joint. If you believe that you might be at risk of developing a bunion, contact a podiatrist who can help you either prevent or treat a bunion.
If you are suffering from bunion pain, contact Sarah Urton, DPM of Kitsilano Foot and Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Vancouver, BC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Congenital Foot Problems
A congenital foot problem is a problem affecting the feet, toes, and/or ankle that a child is born with. Several issues with a child’s feet can occur congenitally. Such problems include clubfoot, vertical talus, tarsal coalition, polydactyly, macrodactyly, and cleft foot. Some of these problems have a genetic basis, with someone in their family history having a gene causing the condition, and some are simply an anomaly.
The following are specifics about a few of these conditions:
- Clubfoot, also called congenital talipes equinovarus or talipes equinovarus, is When the tendons of the foot shorten, the bones are of an unusual shape, and the Achilles tendon is tight, causing an inward and downward pointing of the foot. The soles of the feet might also face each other. In most cases of clubfoot, both feet are affected. If not treated, the affected child will walk on the sides of their feet or ankles.
- Polydactyly is a condition where the child has more than five fingers or toes on either or both feet. Presentation usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus is where the talus bone forms in the wrong position, other bones in the foot do not line up properly, the front of the foot points up, and the bottom of the foot is stiff, has no arch, and usually curves out. This can occur in one or both feet and if left untreated, can lead to serious disability or discomfort as the child grows.
- Tarsal coalition is when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot. The tarsal bones, located toward the back of the foot and in the heel, are the ones affected. This condition is often present at birth, but signs of the disorder usually come on in early adolescence.
- Cleft foot is a rare condition where the foot has missing toes, a V-shaped cleft, and other anatomical differences. Surgery can often help improve the foot’s function since the heel remains normal and is what is most needed for walking. The main issues with this affliction are whether the affected foot can fit into a shoe and the shape and appearance of the foot.
- Macrodactyly is when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue. Having this condition makes it harder for the child to use the affected foot for certain activities.
Accessory Navicular Syndrome

The accessory navicular is an extra bone or piece of cartilage on the inner side of the foot, just above the arch. This is congenital, or present at birth. Most people do not have this as it is not part of the normal bone structure. People who have this condition are often unaware that they have it, especially if it does not cause problems. However, some people with this extra bone develop accessory navicular syndrome, which is painful. The pain comes from aggravation to the bone or posterior tibial tendon that can come from trauma (like a foot or ankle sprain), chronic irritation (from friction from shoes rubbing against the extra bone), or prolonged activity or overuse. Many of those with this affliction also have flat feet or fallen arches. Having flat feet puts more strain on the posterior tibial tendon, and this can cause inflammation or irritation of the accessory navicular. Symptoms of this syndrome usually appear in adolescence when the bones are mature and cartilage develops into bone. Signs and symptoms of this condition include a visible bony prominence with redness or swelling on the inside of the foot, just above the arch, and a vague pain or throbbing in the midfoot and arch areas, usually after periods of activity. If you or your child have pain in this area of the foot, please see a podiatrist for proper diagnosis and appropriate treatment.
Congenital foot problems require immediate attention to avoid future complications. If you have any concerns, contact Sarah Urton, DPM of Kitsilano Foot and Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Congenital foot problems are deformities affecting the feet, toes, and/or ankles that children are born with. Some of these conditions have a genetic cause while others just happen. Some specific foot ailments that children may be born with include clubfeet, polydactyly/macrodactyly, and cleft foot. There are several other foot anomalies that can occur congenitally. What all of these conditions have in common is that a child may experience difficulty walking or performing everyday activities, as well as trouble finding footwear that fits their foot deformity. Some of these conditions are more serious than others. Consulting with a podiatrist as early as possible will help in properly diagnosing a child’s foot condition while getting the necessary treatment underway.
What are Causes of Congenital Foot Problem?
A congenital foot problem is one that happens to a child at birth. These conditions can be caused by a genetic predisposition, developmental or positional abnormalities during gestation, or with no known cause.
What are Symptoms of Congenital Foot Problems?
Symptoms vary by the congenital condition. Symptoms may consist of the following:
- Clubfoot, where tendons are shortened, bones are shaped differently, and the Achilles tendon is tight, causing the foot to point in and down. It is also possible for the soles of the feet to face each other.
- Polydactyly, which usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus, where the talus bone forms in the wrong position causing other bones in the foot to line up improperly, the front of the foot to point up, and the bottom of the foot to stiffen, with no arch, and to curve out.
- Tarsal coalition, when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot.
- Cleft foot, where there are missing toes, a V-shaped cleft, and other anatomical differences.
- Macrodactyly, when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue.
Treatment and Prevention
While there is nothing one can do to prevent congenital foot problems, raising awareness and receiving neonatal screenings are important. Early detection by taking your child to a podiatrist leads to the best outcome possible.
If you have any questions please feel free to contact our office located in Vancouver, BC . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.